Figure 1 Model of a SpineShape implant: the screws are anchored into the spinal column while the rods connect the screws. Image by S. Freudiger
INDICATIONS OF SPINESHAPE
What is SpineShape?
SpineShape is an implant used to perform an innovative procedure called “dynamic stabilization”. This technique stabilizes the vertebral column by controlling uncoordinated (and therefore painful) movements of the spine and unloading the vertebral column of some of the weight that it must carry. The resulting dynamic stabilization of the column and the reduction of the forces that it must bear helps treating different spinal affectations and favours the reduction of the pain associated with those.
When do we use SpineShape?
The vertebral column —also known as spine— is a group of bones (vertebrae) that constitutes the body’s backbone. It is extremely important because it protects the spinal cord (a collection of nerves that connects the brain with most of the body), but also because it carries the body’s weight and allows movement, balance and strength.
Because of its pivotal role in everyday life, affectations in the spine can heavily impact our day-to-day life and determine our quality of life. Some of these affectations may originate from congenital disorders, from injuries or due to aging. In the past, but also currently, a common surgical approach to treat these affectations has been spinal fusion, a procedure which completely immobilises the affected vertebrae.
SpineShape presents an alternative to fusion; rather than a total immobilization, SpineShape provides a dynamic stabilization of the affected segments, maintaining mobility, reducing the pain and preventing further degradation of the column in the future. Image adopted from www.mayfieldclinic.com
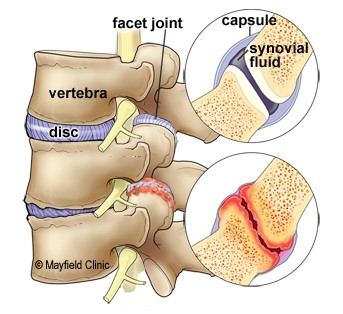
- Discopathy or degenerative disc disease. These terms include conditions in which the anatomy and the function of one or more intervertebral discs are altered. Common examples of a discopathy are disc prolapse or herniation: the soft, central portion of the disc bulges out to the external membrane of the disc due to excessive wear and tear and/or aging2.
- Spondyloarthrosis: a term that encompasses various diseases affecting the joints in the vertebral column, for instance, the joint facet syndrome. This particular syndrome refers to alterations in the posterior facet joints found in the vertebrae that lead to back pain3.
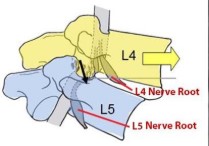
- Degenerative spondylolisthesis; a condition characterized by instability of the spine in which one vertebra “slips” and becomes displaced compared to the adjacent vertebrae4,5. The use of SpineShape is only effective if the displacement is no greater than 25% (Meyerding grade
- Stenosis; a condition in which the spinal canal (the cavity in the vertebral column that contains the spinal cord) is abnormally narrowed due to aging, injuries, or other diseases, among other causes. In consequence, there is an increment in the pressure on the nerves of the spinal cord6.
- Spinal Osteochondrosis or Scheuermann's disease, a disease caused by the interruption of the blood supply of the spine —most commonly during periods of rapid growth— that leads to malformations in the vertebral column. It usually affects teenagers.
- Degenerative scoliosis; a medical condition mainly affecting the elderly population in which the vertebral column presents an abnormal sideways curvature. Although the causes of this condition are not clear, it is associated with progressive degeneration of different structural elements of the spine 7.
- Late adjacent segment syndrome, which refers to degenerative changes found in the vertebrae adjacent to a surgically treated one following the intervention, accompanied by related symptoms like instability, radiculopathy or myelopathy8.
Although less common, SpineShape can also be used as a complement to other types of procedures, like the replacement of damaged intervertebral discs with artificial prosthetics or spinal fusions. Image adopted from www.orthobullets.com
Adaptability of SpineShape
The main body of the SpineShape implant is secured by rods available in three different levels of stiffness, which allows the best fitting depending on the needs of the patient. While the medium-stiffness rod can be used in any case, the stiffest rods are especially recommended for treating osteochondrosis, spondylolisthesis and scoliosis. On the other hand, the most elastic type of rod is especially suitable for the treatment of stenosis, spondyloarthrosis and osteochondrosis. Besides these general indications, Doctors can use additional information from each patient (like the degeneration state of the vertebrae, the age of the patient, their physical condition…) to determine the best level of stiffness in each case. This decision can even be modified in the Operating Room if any additional fact comes to light, as the surgical procedure does not change among the types of rod.
Chart defined by investigating surgeons and Spine Save AG.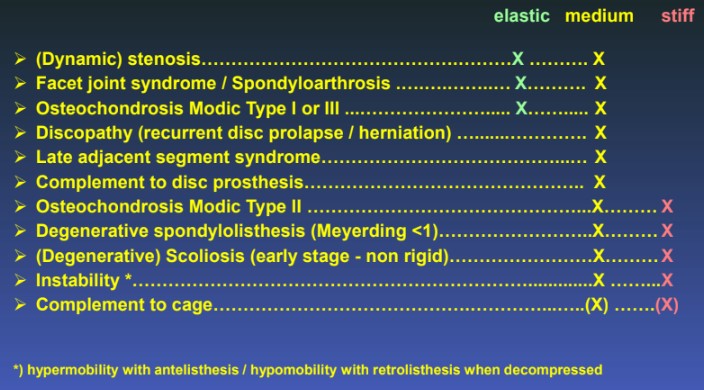
Bibliography
Articles
2. Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology, and the American Society of Neuroradiology. Fardon DF et al.
3. Facet joint syndrome: from diagnosis to interventional management. Perolat R et al.
5. The myth of lumbar instability: the importance of abnormal loading as a cause of low back pain. R. C. Mulholland.
7. Degenerative Scoliosis: A Review. Kotwal S, et al.
8. Adjacent Segment Disease Perspective and Review of the Literature. Saavedra-Pozo, FM et al.
Online Support
1. www.youtube.com/watch?v=2srqmnYxR0E&t=32s
4. www.dictionnaire-medical.net
Other
1. www.spine.org





